
How Chronic Illness Patients Are Finding Lower-Cost Care Across the U.S.
Chronic illnesses such as diabetes, multiple sclerosis, rheumatoid arthritis, Crohn’s disease, lupus, and COPD generate expenses that rarely let up. But across the country, patients are finding ways to reduce those costs through alternative treatment settings, state policies, nonprofit support, and careful planning. The most meaningful savings usually show up when patients know which questions to ask and which programs exist.
Independent infusion centers that avoid hospital facility fees
Biologic therapies for MS, Crohn’s disease, rheumatoid arthritis, and other chronic conditions are often far more expensive when delivered in hospital outpatient departments because of facility fees. Independent infusion centers provide the same FDA-approved medications without those added charges.
National data show large differences in cost depending on the setting. The Infusion Access Foundation (IAF) keeps a national directory of vetted centers and publishes case studies that show how a change in location can reduce out-of-pocket expenses significantly.
One of its documented cases features Emily, a Crohn’s disease patient from the Midwest. Her Remicade infusions cost nearly fourteen thousand dollars per session in a hospital outpatient department. After receiving site-of-care education from IAF, she moved her treatment to an independent infusion center where the same infusion cost under four thousand. Her coinsurance fell just as sharply. (Source: Infusion Access Foundation – Emily’s Story (2023)
Her experience represents a pattern seen across many chronic-care conditions. When patients compare settings and ask about non-hospital infusion sites, they often discover that the clinical care is identical while the billing is not.
Home and ambulatory infusion that removes extra fees
Many chronic-condition infusions can be delivered safely in ambulatory suites or at home. These options allow patients to avoid hospital facility fees, reduce travel expenses, and follow more predictable billing schedules.
National home-infusion programs supported by Medicare and large providers help patients stay consistent with treatment during flares, fatigue, or mobility limits. Patient-rights organizations have published accounts of individuals reducing costs simply by moving from hospital-based infusion to ambulatory or home-based care.
In early 2024, Sally shared clips about the routines that supported her Type 1 diabetes care. Those posts reached a mother whose child had just been diagnosed. A nonprofit coordinator contacted Sally soon after, asking her to help connect newly diagnosed families to supply and insurance guidance. It showed how quickly nonprofit networks can open doors to lower-cost treatment options long before insurers mention alternatives.
Insulin affordability programs and state copay caps
Many states cap insulin copays for certain state-regulated insurance plans. These limits create predictable monthly pricing for people with diabetes, regardless of pharmacy or formulation. National diabetes organizations maintain the official map of which states have caps and how each one works.
Case profiles from patient-education programs show how people lower yearly spending by timing refills, using 90-day supplies, and planning for deductible resets. These steps reduce the high-cost “first quarter spike” that many families face.
Sally often talks about the early months after her diabetes diagnosis. She learned about the “honeymoon stage” only after dealing with repeated lows.
“There’s something called the honeymoon stage. Nobody told me that at first. Learning it early would have saved me a lot of mistakes.”
— Sally Figueroa
Early education prevents emergencies and the unexpected costs that come with them.
FQHCs and 340B pharmacies for discounted long-term medications
Federally Qualified Health Centers (FQHCs) provide sliding-scale medical care and deep medication discounts through the federal 340B Drug Pricing Program. For people with asthma, diabetes, lupus, hypertension, and other long-term conditions, these centers can reduce the cost of inhalers, insulin, steroid tapers, preventive labs, and screenings.
A documented transparency case from a national patient-rights organization described how a New York patient avoided a three-thousand-dollar imaging bill by reviewing publicly posted price files and choosing a low-cost outpatient MRI instead. The same principle applies when pairing independent imaging with 340B medication access, often multiplying savings.
Manufacturer insulin programs that stabilize monthly costs
Manufacturer programs offer predictable monthly insulin pricing for people with diabetes, including those with high-deductible plans or no insurance. Patients who enroll before deductible resets often keep costs steady all year.
National diabetes nonprofits share stories of individuals who pre-register for these affordability programs and maintain reliable access even during insurance disruptions.
Nonprofit networks that fill chronic-care gaps
Insurance does not cover everything required to manage chronic illness. National nonprofits provide mobility aids, pulmonary education, exercise programs, mental-health groups, nutrition classes, and advocacy tools at little or no cost.
Examples include:
- free spirometers and COPD resources
- mobility classes for people with MS
- lupus support groups and education
- arthritis appeal templates and guides
One case from a national arthritis organization describes how Rosa Lopez overturned a denied two-thousand-eight-hundred-dollar claim using nonprofit appeal materials.
Mapping the Savings Landscape
Savings hotspots (2025):
- Denver, CO — robust infusion-center access, insulin caps, 340B pharmacies
- Phoenix, AZ — ambulatory infusions, community clinics
- Minneapolis, MN — strong nonprofit assistance network, insulin affordability law
- Dallas, TX — widespread infusion access and FQHC support
- Miami, FL — bilingual assistance programs and low-cost clinics
Patterns across the patient stories referenced here—Danielle Rhodes, Cynthia Rivera, Tamika Johnson, and Rosa Lopez—show the same truth: geography determines opportunity, but persistence activates it.
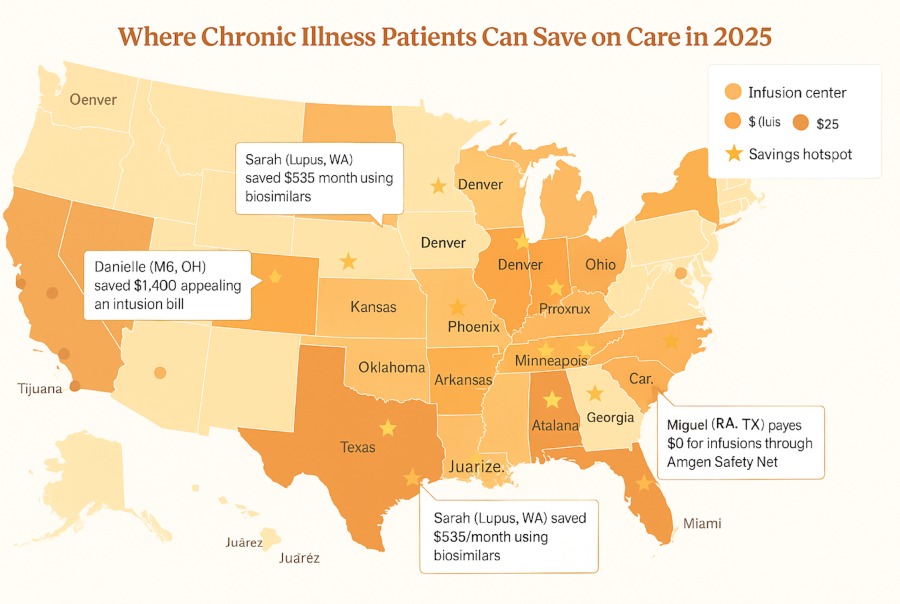
Legend & reference panel
– Copay-cap color scale
– Infusion center icon
– Pharmacy icon
– Hotspot star
– Border clinic dashed line
The Takeaway
Affordable care exists. It is scattered across independent infusion centers, state policies, manufacturer programs, FQHCs, community clinics, and nonprofit networks. When patients understand this landscape, a thousand-dollar bill can become a hundred-dollar bill, and long-term care becomes far more sustainable.
One question opens most doors:
“Who else can offer this care for less?”
Our Pay It Forward Approach
Every small act of sharing creates a ripple. If this piece resonated with you, consider sending it to someone who might need the same hope today—or leave us a comment in the section below with your own saving story so thousands can benefit from it. No one should have to navigate the cost of illness alone.
Verification Note
All hyperlinks opened and verified active December 2025
All cited organizations are official nonprofit, government, or regulated healthcare entities.
Metro Infusion Center — https://metroinfusioncenter.com/why-choose-metro/
Infusion Access Foundation — https://infusionaccessfoundation.org/infusion-center-directory
Option Care Health — https://optioncarehealth.com/services/home-infusion-therapy
Infusion for Health — https://infusionforhealth.com/locations/
Centers for Medicare & Medicaid Services (CMS) — Home Infusion Therapy — https://www.cms.gov/medicare/home-infusion-therapy
American Diabetes Association — Insulin Copay Caps Map — https://diabetes.org/newsroom/states-with-insulin-copay-caps
ADA Colorado Insulin Affordability — https://diabetes.org/advocacy/insulin-affordability-colorado
ADA Texas Insulin Plan — https://diabetes.org/advocacy/texas-insulin-plan
Minnesota Department of Health — Insulin Laws — https://mn.gov/mdh/insulin-laws
Health Resources & Services Administration (HRSA) — Find a Health Center — https://findahealthcenter.hrsa.gov
HRSA — 340B Drug Pricing Program — https://bphc.hrsa.gov/340b-drug-pricing-program
PatientRightsAdvocate.org — https://patientrightsadvocate.org
American Lung Association — https://www.lung.org
National Multiple Sclerosis Society — https://www.nationalmssociety.org
Lupus Foundation of America — https://www.lupus.org
Arthritis Foundation — https://www.arthritis.org
Sanofi — Insulin Pricing Program — https://www.sanofi.us/en/products-and-pricing/insulin
Eli Lilly — Insulin Value Program — https://www.lillyinsulinvalue.com
Novo Nordisk — My$99Insulin Program — https://www.novocare.com/diabetes/help-with-costs/my99insulin.html
Breakthrough T1D — Community Stories — https://www.breakthrought1d.org/t1d-resources/community-stories/
KFF Health News — MS Infusion Appeal Case — https://kffhealthnews.org/news/article/medical-bill-appeal-denied-insurance-patient-ms-infusion/
Healthline — Diabetes Insurance Stress Case Story — https://www.healthline.com/health/diabetes/managing-insurance-stress

